Medical Background
Calcium a basic necessity throughout pregnancy & lactation
• Pregnancy and lactation represent a significant physiological stress on maternal skeletal homeostasis. Approximately 30 grams of maternal calcium is lost during pregnancy and 300 mg per day during lactation.
Optimum calcium intake:NIH consensus statement, 12(4): 1-31(1994)
• Breast fed babies of mothers with lower calcium intakes also receive less calcium.
Calcium levels in maternal milk Br.J.Nutr, 1998:79; 501-507
• Six months of breast feeding is associated with 5.1% bone mineral density (BMD) loss.
Changes in bone density with lactation, JAMA, 1993:269;3130-3135
• In pregnancy, demand for calcium is high (RDA – 1200mg).
92% of the Indian pregnant women take low calcium in diet than RDA Asia Pac J Clin Nutr.2004;13(Suppl):S97.
RDA of Calcium
• Children (1-9 yrs) – 400 mg
• Children (10-15 yrs) – 600 mg
• Adolescents (16- 18 yrs) – 500 mg
• Men – 400 mg
• Women – 400 mg
• Pregnancy and Lactation – 1000 – 1200mg
• Menopausal Women – 1500 mg
• Osteoporosis – 1500 mg
ICMR (Indian council of Medical Research)
Different calcium salts provide different amount of elemental calcium
• Calcium lactate – 13%
• Calcium gluconate – 9%
• Calcium phosphate – 23%
• Calcium citrate – 22%
• Calcium carbonate – 40%
• Calcium aspartate – 20%
• Calcium orotate – 11%
Calcium Carbonate ‘The Gold Standard Calcium’
• Calcium carbonate offers highest elemental Calcium of all Calcium salts.
• Calcium carbonate is the world’s most preferred and most commonly prescribed Calcium salt.
• Calcium carbonate is time tested, safe, effective and most established for therapeutic efficacy in pregnancy.
According to study report published in “New England Journal of Medicine” it was concluded that 39% was absorbed from calcium carbonate.
The best way from the pharmacological point of view of supplementing calcium is in its carbonate form.
Calcium Bioavailability
The amount of drug which reaches the systemic circulation and is available at the site of action
“Bioavailability depends on incorporation of absorbed calcium into bone”Journal of the American College of Nutrition, 2000;19(2): S 109-136
Calcium absorption enhancers
• Vitamin D
• Magnesium
• Lysine
Vitamin D in calcium absorption
Vitamin D stimulates no of proteins (calbindin a intracellular protein that carries calcium across the intestinal epithelial cells) involved in transporting calcium from the lumen of the intestine across the epithelial cells into blood.
• Increases Calcium absorption by 30-80%
• Stimulates bone mineralization
Magnesium
Sources: Nuts, legumes, dark green leafy vegetables
RDA
• Children: 80-130mg
• Adults: 250-300mg
• Pregnancy: 350-400mg
75% population worldwide does not consume the RDA of magnesium.
Role of Magnesium in calcium absorption and utilization
Magnesium deficiency affects calcium homeostasis
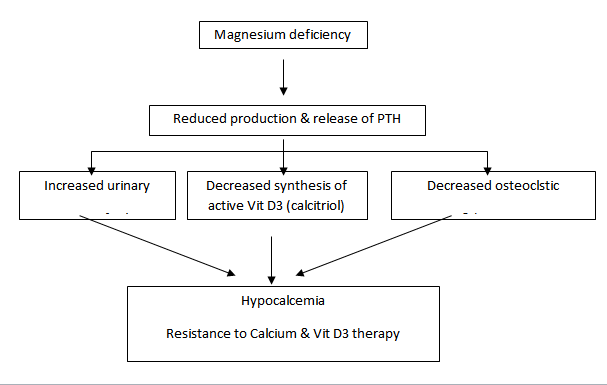
Therefore calcium intake needs to be balanced with Magnesium
Thus magnesium
• Increases Calcium absorption
• Regulates Calcium metabolism
• Reduces urinary Calcium excretion
• Prevents formation of calcium oxalate stones
Supplementation with Calcium alone is never enough
Inadequate intake of magnesium greatly reduces the absorption, utilization and homeostasis of calcium.
Magnesium is a vital key to Calcium & Vitamin D3 utilizatio
“ Normocalcemia cannot be maintained until the deficit of Magnesium is corrected”
Role of L-Lysine in calcium absorption
• Lysine helps the body to absorb and conserve Calcium
• Lysine is required for formation of collagen a substance important for bones and connective tissues.
Bone friendly minerals (Zinc, Boron, and Copper)
Zinc: Zinc is required for bone mineralization.
(Alkaline phosphatase an enzyme responsible for mineralization is a zinc dependent metallo-enzyme. Thus, zinc supplementation helps in better mineralization).
Boron: Boron is essential for healthy bone and joint function because it affects the balance and absorption of Calcium, magnesium & phosphorus.
Boron reduces excretion of calcium by 44%
Copper: Important micronutrient, required for maintaining bone health.
(Copper is essential part of wide range of proteins and enzymes. One of these protein is collagen, a structural protein found in connective tissue like bones, thus is necessary for healthy bones.)
Complications of Pregnancy
PIH – Pregnancy induced hypertension – Development of significant hypertension after 20 weeks of gestation in previously normotensive women.
Pre-Eclampsia – PIH accompanied by proteinuria, headaches and edema of lower extremities.
Preterm Birth – Birth that takes place before 38 weeks of gestation.
Miscarriage – End of pregnancy(20 weeks0 at the stage when the fetus is incapable of surviving.
IUGR(Intra uterine growth retardation) – Growth of the fetus with in the uterus is not as per the standards.
Calcium in reducing the risk of PIH:
During pregnancy blood volume increases but diameter of the blood vessels remains the same. Increased blood flow creates pressure on the walls of the blood vessel which leads to PIH, Pre-Eclampsia and Eclampsia.
Calcium helps in the production of nitric oxide which maintains the vasodilation, which is important for normal pregnancy.
Magnesium in reducing the risk of PIH:
Magnesium amplifies the release of prostacyclin, which acts as a vasodilator.
Thus calcium and magnesium together exerts synergistic effect in reducing the risk of PIH / Pre-Eclampsia / Eclampsia.
Clinical Evidences
Reduces PIH & Pre-eclampsia
“Magnesium sulphate reduces the risk of Pre-eclampsia and maternal death” Cocharane Database Syst Rev,2003;(2):CD000025, Update of Cochame Database Syst rev,2000;(2):Cd000025
Reduces Preterm Birth
“Magnesium Therapy is necessary in cases of Preterm Birth and Pre-eclampsia” Medical Science Monitor,2001 Mar-Apr;7(2):332-40
Prevents IUGR & Miscarriages
“Oral supplementation of Magnesium during pregnancy reduces growth retardation, miscarriage and foetal preterm birth”Nutrition and health 1988;6(2):69-88 By:Wynn A Wynn M
Ensures Healthy Maternal & Foetal Development
“Magnesium Supplementation during pregnancy has a significant influence on foetal and maternal morbidity”Br J Obstet Gynaecol,1988 Feb;95(2):120-5
Role of Ca & Mg in Kidney stone formation
• Low intake of magnesium increases urinary calcium excretion with increased risk of kidney stone formation. Jnl. Of Nutrition,118:729-734,1988. NIH Consensus Statement, June 6-8:12(4):p 16,1994
• Magnesium promotes the absorption & metabolism of Calcium and keeps them soluble in urine & prevents them from turning into solid stone.Nutrition Almanac (Revised Edition) Pg-73-74, Nutrition Search, Inc)
